Click here to download the PDF
1. Purpose
This document provides guidance for healthcare professionals managing situations where The Insides Tube has migrated into the distal intestine. It is intended to support safe and effective clinical decision-making, helping to minimise the risk of patient harm. The information contained here should be used as supplementary material alongside the clinical judgment and expertise of the treating healthcare team.
2. Scope
This document applies to specialised colorectal and/or gastroenterology multidisciplinary teams that manage patients who are performing chyme reinfusion therapy with The Insides System. This includes Colorectal surgeons, Gastroenterologists, Stomal therapy nurses who have been trained to install The Insides System, troubleshoot, and support patients’ day to day with using the device.
There is a low risk that The Insides Tube may migrate into the intestine, generally due to peristalsis. This document will provide a trained healthcare professional with guidance on the safe and effective management of such occurrences, including the process to safely remove The Insides Tube.
3. Definitions
Tube Migration - If The Insides Tube migrates into the distal intestine, it either gets completely drawn in or it partially drawn in with The Insides Pump stopping it from being drawn in any further.
Common terms:
• Tube or catheter ingress
• Tube or catheter displacement
• Tube or catheter pushed in
• Tube or catheter sucked in
• Tube or catheter migration
• Tube or catheter completely disappears
Tube - The Insides Tube
Pump - The Insides Pump
4. Responsibilities
It is the responsibility of the healthcare professional managing the day-to-day care of the patient to provide all the training to the patient, so they are able to manage and troubleshoot the device themselves. During this initial training period, the patient should be supplied with the contact numbers of their healthcare team, so they know who to call in an emergency.
5. Identification and Clinical Management Steps
Note: If a patient is at home in the community, the patient must be reviewed face to face by their healthcare professional; do not let the patient attempt the removal of the Tube themselves.
The following procedure should be completed by a trained health care professional and we suggest having a second healthcare professional assisting:
1. Ensure the patient is comfortable
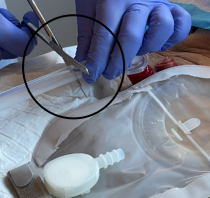
2. Stop the tube from migrating further into the intestine by securing with metal forceps, or other suitable means. If the Pump is the only accessible component, this can be secured, however do not pull on it.
3. Administration of antispasmodic medication is recommended. Be aware of the medication’s onset of action.
4. If the Pump is accessible and is still attached to the Tube, DO NOT REMOVE IT from the Tube.
5. If the Tube is still visible:
a) Suggest use of metal forceps so a firm grip of the Tube can be achieved.
b) Place the forceps around the Tube and pull slowly and consistently. This may take several minutes.
i. Ensure the retention sleeve comes with the Tube. This is where the second healthcare professional may be necessary to manipulate/guide the retention sleeve through the fascial opening either digitally or with a second set of metal forceps
ii. If the Tube feels like it is suctioned in place, fill a ‘catheter tip syringe’ with potable water or saline and administer this down the tube so that it can trickle out of the bulbous end and release the suction.
c) Once out, discard this Tube and replace with a new tube so the patient can continue chyme reinfusion. Prior to inserting a tube, evaluate the patients facial opening to ensure that the tube will not migrate into the intestine. A radiological study may need to be performed to ensure that there is no damage to the intestine. Follow the instructions for Tube insertion in The Insides System Setup Guide for Healthcare Professionals. A video of a Tube insertion is available on the Training Hub (www.theinsides.co/training-hub/home)
d) Take this opportunity to refresh information to the patient about being mindful of vigorous exercise and any abdominal-centric movements such as bending over for long periods of time
e) Once the intervention is complete, report the incident to your local distributor of The Insides System and/or The Insides Company
6. If the Tube is not visible:
a. Radiographic imaging can be used to locate the Tube, Retention Sleeve and Pump
b. Endoscopic removal can be the safest option depending on the location of the Tube
i. ENSURE the Retention Sleeve is removed at the same time as the Tube is removed
c. Once out, discard the Tube
i. If the Tube removal was difficult or there is evidence of bowel injury, we recommend re-imaging the distal bowel with contrast before recommencing chyme reinfusion therapy.
ii. If the Tube removal was routine with no abnormalities seen during the endoscopic intervention, replace with a new Tube so the patient can continue chyme reinfusion. Follow the instructions for Tube insertion in The Insides System Setup Guide for Healthcare Professionals. A video of a Tube insertion is available on the Training Hub (www.theinsides.co/training-hub/home)
d. Take this opportunity to refresh information to the patient about being mindful of vigorous exercise and any abdominal-centric movements such as bending over for long periods of time
e. Once the intervention is complete, report the incident to your local distributor of The Insides System and/or The Insides Company
6. Training and Education
• The Insides Company Clinical team are available for refresher training, complex patient management discussions, and technical support. Please contact them on clinical@theinsides.co or support@theinsides.co
• The Insides Company Training Hub contains up-to-date information, documents for download, and training videos. www.theinsides.co./training-hub/home
Exclusion
The Insides® Company maintain a clinical registry for all patients that use (any form of) CRT. Patient consent is required to enter the patient’s de-identified data. The objective of the Registry is to track patients weaning off PN and EN, increasing their oral feeding and CRT, and safety and efficacy of the device. Submission of patient data is not mandatory for use of The Insides® System but is recommended to provide on-going quality assurance.
Due to the anatomy of the EAF, the choice of feeding tube for use in CR requires careful consideration.
For patients who have been defunctioned for >6 months
For patients who have been defunctioned for <6 months
Things to remember,

Chyme (kaɪm) is the medical term for the brown/green/yellow fluid that comes from your fistula or stoma. It is the watery or pulpy liquid you see in your ostomy appliance. Chyme is made up of all the food and fluids that you eat and drink, plus the digestive juices that your body adds to help breakdown food. Chyme keeps you hydrated, nourished, and your body functioning.
You have a fistula or stoma somewhere along your small intestine. This means chyme leaves your body earlier than expected and does not pass through the rest of your intestines where some of it would normally be absorbed. This puts you at higher risk of becoming dehydrated and malnourished.
Chyme reinfusion therapy is a treatment method for patients like you with fistulas and stomas. Chyme reinfusion therapy involves returning chyme from your ostomy appliance back into the rest of your intestines through the opening of your fistula or stoma. Returning chyme to your body gives the rest of your intestine the chance to absorb the valuable nutrients to keep you hydrated and nourished.

Research shows that chyme reinfusion therapy has benefits for maintaining your gut health, keeps you hydrated and well-nourished, and better prepares your intestines for fistula or stoma reversal.
Performing chyme reinfusion therapy can:
• Keep the remaining part of your intestine working and rehabilitated. Without chyme reinfusion therapy, it will start to shrink due to lack of use. Reinfusing chyme keeps your intestine healthy so that it will begin working immediately after your reversal surgery.
• Rehabilitate your large intestine with healthy bacteria (microbiome) to help your body breakdown and absorb chyme.
• Maintain the health of your entire digestive tract, keeping you hydrated. Chyme reinfusion therapy may reduce the need for intravenous (IV) fluids. Chyme contains electrolytes, such as salt, which will help keep your system balanced and reduces kidney damage.
• Help you to have regular bowel movements again.
• Reduce the amount of time you might spend in the hospital.
• If you need IV nutritional support, reinfusing chyme encourages your liver to keep working, making digestive enzymes needed to breakdown food, reducing long-term liver damage.
Performing Chyme Reinfusion Therapy
Chyme reinfusion therapy can be done two ways: manually or with a medical device called The Insides® System.
If performing manual chyme reinfusion, a nurse will insert a tube into the downstream hole of your stoma. The chyme is taken out of your ostomy appliance, strained, and drawn up into a syringe. It is then syringed down a tube multiple times a day.
The frequency at which the nurse needs to perform this depends on how much chyme you pass into your ostomy appliance and how often you would normally empty it.
Alternatively, chyme reinfusion therapy can be done using The Insides® System (explained overleaf).
Chyme reinfusion therapy can be done two ways: manually or with a medical device called The Insides® System.
If performing manual chyme reinfusion, a nurse will insert a tube into the downstream hole of your stoma. The chyme is taken out of your ostomy appliance, strained, and drawn up into a syringe. It is then syringed down a tube multiple times a day.
The frequency at which the nurse needs to perform this depends on how much chyme you pass into your ostomy appliance and how often you would normally empty it.
Alternatively, chyme reinfusion therapy can be done using The Insides® System (explained overleaf).
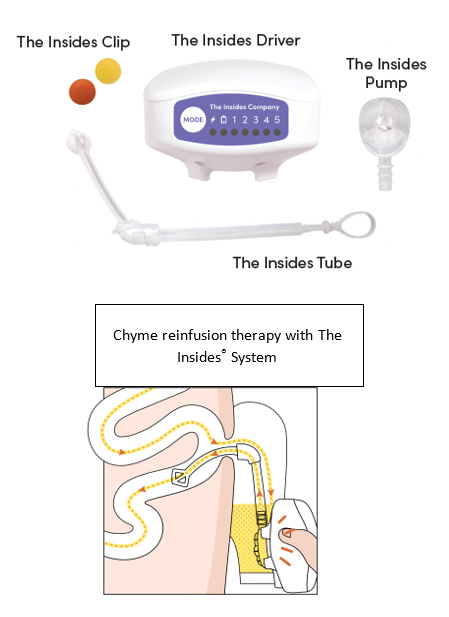
The Insides® System is a medical device that helps you perform chyme reinfusion therapy by yourself. The device is made up of three parts:
• The Insides® Tube (Tube) is placed in your fistula or stoma’s downstream intestine by a healthcare professional and sits inside your ostomy appliance. The Tube is changed every month by your healthcare professional; otherwise, it remains in the stoma throughout refeeding. Although you will be aware of the Tube, it will not be uncomfortable.
• The Insides® Pump (Pump) is a device that slides onto the end of the Tube and is replaced every 2-3 days when changing your ostomy appliance. The Pump sits submerged in the chyme in your ostomy appliance.
• The Insides® Driver (Driver) is a handheld device that you use throughout the day to actively pump chyme from your ostomy appliance into the lower intestine through your fistula or stoma.
The following information will guide you on what you to expect while using The Insides® System.
The First Week
It takes approximately one hour to set up The Insides® System and teach you how to use it. This can be done in a hospital, at home, or in a health clinic.
You will only use the device once or twice a day in the first week to minimise lower tummy discomfort, allowing your intestine to rehabilitate slowly. Your intestine has shrunk while it has been out of use. Putting your chyme down it again is like waking it back up. The first week is the hardest week due to this rehabilitation and it can be uncomfortable until you have had your first few bowel movements. You will discard all remaining chyme in your ostomy appliance into the toilet.
In addition to this, you will also be learning how to change your ostomy appliance with the tube in place. Your stoma nurse is there to support and help you modify how you change your ostomy appliance. Learning to chew your food more and avoiding overly fibrous food will also be a learning process. Please be reassured it does get easier after the first week!
Weeks Two and Three
You will likely have your first bowel movement by the end of your first week. By now, your body should be used to pumping chyme, and your lower tummy discomfort should be disappearing.
You should now be able to pump more often throughout the day. Pumping more often means you will have more bowel movements. Slowly increase the number of times you pump each day based on your comfort level. If you have questions about how much you should pump, speak with your healthcare team.
The Fourth Week
You will arrange an appointment with your healthcare team to change your tube and see how you're doing. You should be feeling comfortable with the device, pumping more often throughout the day, and having regular bowel movements. Based on your progress, your surgeon and healthcare team will be able to tell you how long you will have The Insides® System for.
Your healthcare team will help with your care by providing The Insides® System for your treatment; they have been trained in how to use The Insides® System. Your healthcare team can provide you with the information needed to use The Insides® System safely and effectively.
To prepare for chyme reinfusion therapy using The Insides® System, you will need:
• A positive attitude and commitment to your health.
• To make some small modifications to your diet so that The Insides® Pump will work properly.
• To chew your food well and drink plenty of water.
Set-up a routine for yourself as early as possible to ease the transition into reinfusing your chyme. The following guidance comes from patients that have used the System before you, who want to ensure you have a good experience in your first week. You will become an expert by experience very quickly.
• Find the most comfortable position for you to hold the Driver. You will be completing multiple reinfusions throughout the day so it must be comfortable for you.
• Ensure you are getting enough sleep at night. Forgo a reinfusion to get quality sleep.
• Continue taking your prescribed medication and speaking to your health care team when your output/chyme is starting to get too thick to pump. This is expected, and they will guide you on how to keep it thin.
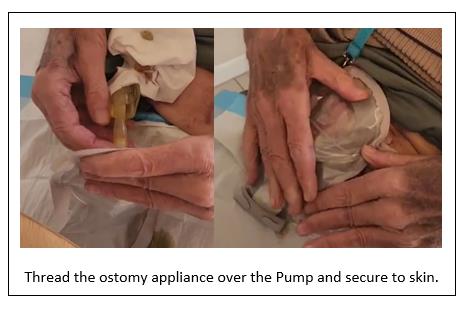
• Practice many times, with supervision from your stoma nurse, changing your ostomy appliance. Threading the ostomy appliance over the Tube takes practice to not accidently pull it out.
• Ensure you feel confident to reinfuse your chyme and safely change your ostomy appliance before discharge
• Your healthcare team will likely give you a laboratory form to complete renal bloods every 1-2 weeks, once you’re home
• 1st day: - reinfuse your chyme one to three times only. About 80 – 100mls each time
• 2nd day: reinfuse your chyme two to four times only. About 80- 100mls each time
• 3rd day: reinfuse your chyme two to four times only. About 100mls – 200mls
o It is the 3rd day - change the Pump and your ostomy appliance
• 4th day: reinfuse your chyme three to five times
• 5th day: continue increasing volume and frequency each day if there is no discomfort, minimal reflux, and pain
• 7th day: You will start to feel confident about reinfusing your chyme about now so your healthcare team will start to reduce your anti-motility medication and your IV nutrition (if you required this)
• By 8 - 14 days, you will likely be reinfusing at least 90% of your chyme each day
When you look down at your stoma or fistula, you should be able to see the Retention sleeve, the Tube, and the Pump.
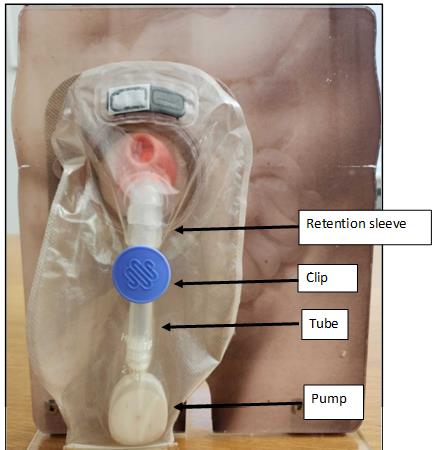
If you notice that it looks different, for example.
· the Tube is sitting at the bottom of the bag or
· you can’t see the Retention sleeve or Tube anymore
Please call your healthcare professional urgently


Efficient Refeeding
1. Reinfuse chyme when The Insides® Pump is completely submerged in chyme, reinfuse little and often.
2. Make sure the pump is changed at least every 3rd day.
3. If you’re experiencing nausea, bloating, and/or stomach cramps – reduce the speed and slowly reinfuse. Only reinfuse 1-2 times per day under the guidance of your health care professional until it resolves. Discomfort will reduce over time, if it continues for longer than 2 weeks, please contact your health care professional.
4. Release excess wind in the ostomy appliance. Press out the wind via the opening at end of pouch or uncoupling the pouch from the base plate.
5. Do not let the ostomy appliance overfill. Reinfuse once you see The Insides® Pump is submerged.
6. Do not refeed chyme which has been sitting in the ostomy appliance for longer than 12 hours. Measure and discard this chyme.
7. There will be approximately 20ml of chyme sitting in the bottom of the ostomy appliance when you finish refeeding due to it sitting below the level of the Pump. As you become more independent, you will be able to fold up the bottom of the ostomy appliance and refeed it or you may choose to discard it.
8. Charge The Insides® Driver when the lightning bolt flashes amber. It will take 4 hours.
9. Ensure you fill in the logbook every day and take it with you to show your healthcare team.
Troubleshooting
1. If the tube falls out - contact your health care professional that is monitoring you on this device, do not replace The Insides® Tube yourself. Please take the Tube in a Ziplock bag with you to the appointment.
2. If you’re experiencing reflux around The Insides® Tube it does not cause harm but will increase the reinfusing time. Reflux is expected when you are rehabilitating the distal bowel.
a. Use the lowest speed that moves the chyme through The Insides® Tube.
b. Reinfuse a little and often to allow the intestine to absorb the chyme that has been pumped.
c. You may be constipated downstream – under the guidance of your health care professional, ensure you are reducing your anti–motility drugs i.e. Loperamide.
d. If reflux continues, please contact your health care professional.
3. If chyme is not moving up the tube, there could be several reasons:
a. Blocked pump: - Change The Insides® Pump. Avoid stringy fibrous food which can block The Insides® Pump.
b. Ensure The Insides® Pump is fully submerged in the chyme.
c. If your chyme is too thick, discard into the toilet and work on thinning your output for the next reinfusion. Drink a glass of water or cup of coffee.
d. The Insides® Driver – Ensure all speeds have been tried for a minimum of 30 seconds each, sometimes the thicker consistency’s move slowly up The Insides® Tube.
e. Not coupled correctly – Ensure the flat surface of The Insides® Pump has been cleared of debris and intuitively couple The Insides® Driver with The Insides® Pump through the ostomy appliance. Carefully hold The Insides® Driver up and The Insides® Pump should remain coupled. This demonstrates they are coupled effectively.
f. The Insides® Driver bounces off The Insides® Pump – This can happen at speed 5 when the chyme is too thick or if The Insides® Pump is blocked.
Dietary Guidelines for Patients
This document should be used as a guide only and provides suggestions on foods that will make your chyme work efficiently with the Pump.
For dietary advice specific to your condition, please consult with your Dietetics team
• Eat slowly and chew your food well.
• Swallowing air while eating can increase wind (e.g., Carbonated drinks)
• Avoid drinking through a straw or chewing gum.
Foods to avoid
(Because they block The Insides® Pump more readily)
• Sweetcorn
• Nuts and seeds (smooth nut butters are ok) (including baked into foods like muffins, cakes and chocolate)
• Coleslaw
• Popcorn
• Stringy fruit & vegetables (e.g. celery, lettuce, including baked into foods like frittata)
• Coconut
• Pineapple
• Mango
• Peas
• Dried fruit
• Raw vegetables with skins (e.g. Potato skins, onion, tomato)
• Wholegrains
• Pith (e.g. from oranges & mandarins)
• Tough pieces of meat that require a lot of chewing
Foods that can increase wind
• Green leafy vegetables
• Pulses (e.g. peas, beans, lentils)
• Onions
• Garlic
• Fizzy drinks
• Beer
• Brassicas (e.g. broccoli, cauliflower, cabbage)
• Asparagus
Foods that will cause watery or increased output
• Alcohol
• Caffeine containing drinks e.g. coffee
• Fruit juice or sugary drinks
• Green leafy vegetables
• Fatty foods
• Fish
• Onions
• Spicy foods
• Raw vegetables
• Chocolate
Contact details
Your Hospital: _____________________________________
Your Surgeon: _____________________________________
Your Stoma Nurse: _________________________________
Email: ______________________________________
Telephone: __________________________________
After-hours urgent contact:
_________________________________
_________________________________
I started The Insides System on: ____ / ____ / ____
Serial number of your Driver (Located on the back of your Driver):
____________________

My Tube needs changing: ____ / ____ / ____
Contrast Imaging of Distal Intestinal Tract
Prior to commencing chyme reinfusion therapy the patient’s distal intestine must be checked to ensure patency. A method of doing this is contrast imaging.
Selecting the Correct Tube Size
The Insides System contains two sizes of The Insides Tube, 28 Fr and 22 Fr. As a general guide:
If the Clinician determines that neither the 28 Fr or 22 Fr tube sizes are appropriate, a minimum 20 Fr balloon retained tube is recommended. Please note, a balloon retained tube with an ENFitTM connection does not couple with The Insides Pump.
The Insides Tube 28Fr tube is recommended when applicable. If the 28Fr does not fit, smaller tubes can be used to reinfuse small boluses to rehabilitate the intestine. After a short period of intestinal rehabilitation, the patient may be able to transition to a version of The Insides Tube or transition from the 22 Fr to the 28 Fr Tube.
Parastomal Hernia
If a patient has a parastomal hernia, caution is needed when inserting the tube. Possible bowel kinking can prevent the tube from being inserted and can create a risk of perforation. The increased external length of bowel can prevent the tube from being positioned and anchored correctly. Digitally palpating the distal tract will indicate the direction of distal limb, any narrowing or kinking, and the distance to fascia.
Prolapsed Distal Limb
If the patient has a prolapsed distal limb of their enterostomy or enterocutaneous fistula (ECF), caution is needed when inserting the tube due to the extended, unsupported length of intestine that is external to the body. The Insides Tube is not suitable for this type of patient.
Enterocutaneous Fistulas
If a patient has an ECF, caution and careful clinical decision making are required when selecting the correct tube to use for the patient. Patients may have little or no fascia around the location of tube insertion. Consequently, a retention sleeve or cuff may not prevent the migration of the tube into the distal intestine as it matures. An appropriate tube should be selected and monitored to ensure the migration does not occur.
Ostomy Appliance Selection
The Insides Tube can be used with any ostomy appliance. Initially, it is recommended the patient use a clear ostomy appliance, so it is easy to watch chyme move up the tube and see the volume in the ostomy appliance decreasing. If a tube, other than The Insides Tube, is required initially, then this tube and pump must fit comfortably within the ostomy appliance without any pressure exerted on the tube and The Insides Pump.
Basic Stomal Therapy Principles
The installation of a feeding tube into the patient’s distal limb may increase the size of the stoma on the abdomen. Consequently, it is recommended that the patient’s template on the base plate of the ostomy appliance, is re-measured. This is to ensure there is a clearance of 2 – 3 mm between the enterostomy and the edge of the base plate. This allows for peristalsis and the natural movement of the enterostomy and tube complex to prevent the risk of mucosal erosion due to rubbing on the side of the base plate. It is best to re-measure the patient’s template periodically. The base plate should also be re-measured if there have been any changes as a result of weight gain, weight loss, herniation, or prolapse.
Commencing Treatment with The Insides System
When starting therapy with The Insides System, the patient will spend a short period of time increasing their tolerance to chyme reinfusion therapy, rehabilitating their distal bowel, and slowly introducing oral food. During this period, it is recommended to keep the patient’s parenteral nutrition prescription and anti-motility medication at the same dose. This will allow the patient to become independent with The Insides System and not become overwhelmed with the increase in their output from weaning the anti-motility medication. This will also maintain their nutrition while they are transitioning to reinfuse all of their output and ensure their nutrition is optimised.
*If printing, please print in A3 or larger

Prior to commencing chyme reinfusion therapy the patient’s distal intestine must be checked to ensure patency. A method of doing this is contrast imaging.
The Insides System contains two sizes of The Insides Tube, 28 Fr and 22 Fr. As a general guide:
If the Clinician determines that neither the 28 Fr or 22 Fr tube sizes are appropriate, a minimum 20 Fr balloon retained tube is recommended. please note, a balloon retained tube with an ENFitTM connection does not couple with The Insides Pump.
The Insides Tube 28Fr is recommended when applicable. If the 28Fr does not fit, smaller tubes can be used to reinfuse small boluses to rehabilitate the intestine. After a short period of intestinal rehabilitation, the patient may be ble to transition to a version of The Insides Tube or transition from the 22 Fr to the 28 Fr Tube.
If a patient has a parastomal hernia, caution is needed when inserting the tube. Possible bowel kinking can prevent the tube from being inserted and can create a risk of perforation. The increased external length of bowel can prevent the tube from being positioned and anchored correctly. Digitally palpating the distal tract will indicate the direction of distal limb, any narrowing or kinking, and the distance to fascia.
If the patient has a prolapsed distal limb of their enterostomy or enterocutaneous fistula (ECF), caution is needed when inserting the tube due to the extended, unsupported length of intestine that is external to the body. The Insides Tube is not suitable for this type of patient.
If a patient has an ECF, caution and careful clinical decision making are required when selecting the correct tube to use for the patient. Patients may have little or no fascia around the location of tube insertion. Consequently, a retention sleeve or cuff may not prevent the migration of the tube into the distal intestine as it matures. An appropriate tube should be selected and monitored to ensure the migration does not occur.
The Insides Tube can be used with any ostomy appliance. Initially, it is recommended the patient use a clear ostomy appliance, so it is easy to watch chyme move up the tube and see the volume in the ostomy appliance decreasing. If a tube, other than The Insides Tube, is required initially, then this tube and pump must fit comfortably within the ostomy appliance without any pressure exerted on the tube and The Insides Pump.
The installation of a feeding tube into the patient’s distal limb may increase the size of the stoma on the abdomen. Consequently, it is recommended that the patient’s template on the base plate of the ostomy appliance, is re-measured. This is to ensure there is a clearance of 2 – 3 mm between the enterostomy and the edge of the base plate. This allows for peristalsis and the natural movement of the enterostomy and tube complex to prevent the risk of mucosal erosion due to rubbing on the side of the base plate. It is best to re-measure the patient’s template periodically. The base plate should also be re-measured if there have been any changes as a result of weight gain, weight loss, herniation, or prolapse.
When starting therapy with The Insides System, the patient will spend a short period of time increasing their tolerance to chyme reinfusion therapy, rehabilitating their distal bowel, and slowly introducing oral food. During this period, it is recommended to keep the patient’s parenteral nutrition prescription and anti-motility medication at the same dose. This will allow the patient to become independent with The Insides System and not become overwhelmed with the increase in their output from weaning the anti-motility medication. This will also maintain their nutrition while they are transitioning to reinfuse all of their output and ensure their nutrition is optimised.
THE INSIDES® Driver (driver) should be fully charged before the first use. The charging light will turn ON while the driver is charging and will turn OFF when it is fully charged. The full charge cycle could take up to four hours. After each use of the driver, all accessible surfaces should be wiped down using a damp cloth followed by an EPA recommended disinfectant wipe. Before commencing prepare a clean work station and don gloves.
The patient must have visibility into the ostomy appliance to ensure that THE INSIDES® System is successfully reinfusing chyme. Use a clear ostomy appliance or remove outer lining of the patient's usual ostomy appliance to ensure adequate visibility.
THE INSIDES® Pump (pump) is 35 mm in diameter and will be threaded through template of the ostomy appliance. Therefore, a larger template may need to be cut and a hydrocolloid seal used to protect the exposed skin. If this is not suitable an ostomy appliance with a “lock and roll” closure at the bottom of the bag can be used. In this scenario, the pump will be connected to THE INSIDES® Tube (tube) through this opening.
THE INSIDES® Tube must be inserted by a healthcare professional. The Insides® Tube must be replaced every 28 days.
1. Select the appropriately size feeding tube based on the diameter of the patient’s
stoma.
2. The patient should be resting in a comfortable supine position. Remove the patient's ostomy appliance and wipe away any excess chyme from the area. Only reinfuse chyme that is less than eight-hours old. Store the patient's chyme if this is the first use of THE INSIDES® System.
3. Unpackage the tube. A retention sleeve and guidewire are also provided to aid user comfort and insertion, respectively.
4. Lubricate the tube using 10-20 mL of water-based lubricant as described below:
a. Unfold the arms of the retention
sleeve from the tube.
b. Spread lubricant in front of and
behind the retention sleeve. With adequate force, pull the retention sleeve backward, towards the handle of the guidewire, over the lubricant, then return it to its original position. Continue this until the retention sleeve moves freely. Add more lubricant if it is required. Then, move the retention sleeve towards the bulbous section of the tube. Ensure the retention sleeve is not pulled off.
c. Lubricate the bulbous section of the tube.
d. Set the tube aside on the clean workstation.
5. With additional lubricant, digitally examine the direction of the
distal tract. Palpate the fascia to gauge the approximate length required for the insertion of the tube. If the distal tract is tight or kinked, insert 3-10 mL of additional lubricant.
6. During the examination, the patient may feel some abdominal discomfort. Discomfort is due to the stretching of the intestinal lumen and should be expected. After digitally palpating the distal tract, replace gloves.
7. Collapse the tube's bulbous feature by inserting the guidewire until the base of the tube touches the 'stop' on the guidewire. Pinch the guidewire between the tube and maintain pressure so it stays in place. Ensure that the guidewire's tip is sitting within the nose of the tube and not sticking out through the bulbous section.
8. While the bulbous section is collapsed, use the free hand to guide the tube and insert it into the distal limb. Apply gentle pressure until the bulbous feature of the tube is 10-20 mm past the abdominal fascia. The intestine may not allow the tube to be immediately inserted; it may take up to 60 seconds for peristalsis to help move the tube into place.
9. Firmly hold the tube in place with one hand and remove the guidewire with the other.
10. Allow the tube to settle into its natural position. The tube may move outwards up to 10mm due to peristalsis.
11. Move the retention sleeve up the tube until it sits 1-2 mm away from the stoma. Fold the arms of the retention sleeve over the tube to secure it in place.
Due to differing patient anatomy, the retention sleeve may block the proximal outlet. If this occurs, chyme may leak under the baseplate of the ostomy appliance. If this happens, the retention sleeve can be moved down the tube, away from the stoma.
12. Gently tug on the tube to confirm it is anchored in place.
13. If the tube becomes dislodged, remove it entirely from the patient before reinserting the guidewire into the tube:
a. Move the retention sleeve toward the bulbous feature.
b. Insert lubricant into the Tube.
c. Insert the guidewire into the Tube, beyond the retention sleeve in a single fluid
motion.
d. If the guidewire does not slide beyond the retention sleeve, move the guidewire's tip back into the lubricant, then repeat Step c.
e. Hold the guidewire in place and move the retention sleeve to the centre of the Tube.
f. Return to Step 3.
14. Once the tube is successfully inserted, dispose of the guidewire appropriately.
WARNING: Do not insert the guidewire into the Tube while it is positioned inside a patient - this could result in perforation of the bowel.
NOTE: Peristalsis may move the tube in and out of the stoma slightly. When placed correctly, the tube should not fall out on its own and the retention sleeve will prevent it from being pulled too far into the distal intestine.
1. Connect the pump to the tube. The base of the tube should touch the third ring of the pump outlet to ensure it cannot be accidentally dislodged.
2. Allow the patient or their carer to practise connecting and disconnecting the pump while ensuring that the tube position is not disturbed.
3. Measure the ostomy appliance against the tube and pump. Trim the end of the tube so
that the pump sits 10-20 mm above the bottom of the ostomy appliance when attached.
4. The pump can rotate around the tube until oriented such that the position allows the connecting of the pump to the driver.
A clip is provided to hold the tube in place. Once the Ostomy appliance has been applied, a clip can be attached to the tube from the outside of the bag to help prevent the tube falling out and reduce pulling on the stoma. Choose the clip that will fit around the section of the tube immediately below the retention sleeve. This will depend on the size of the tube and how short the tube is trimmed. Ensure the patient is aware of which clip should be used.
1. Assess the suitability of the patient's chyme from the patient's previous ostomy
appliance.
a. Pinch the ostomy appliance between the thumb and forefinger. Release it quickly to observe the time it takes for the chyme to refill the space. If it is instantaneous, the chyme can be pumped; otherwise, it may be too thick and should be discarded.
b. Chyme sitting for less than eight hours is suitable for pumping; otherwise, it must be discarded.
c. There must be enough volume for the Pump to be fully submerged in the chyme, approximately 70-100 mL.
2. If the patient's chyme is suitable for reinfusing, transfer the chyme into the new ostomy appliance. If not, fill a new ostomy appliance with enough water to submerge the Pump. Water can be used to demonstrate chyme reinfusion to the patient. Ensure the patient understands that they should not add water to the ostomy appliance in any other setting. Secure the ostomy appliance as described above.
1. Ensure the pump is fully submerged in the chyme.
2. Magnetically connect the pump to the driver.
a. Hold the driver and pump in an orientation allowing the user to see the tube. The user should be able to be to see whether chyme is progressing up the tube.
3. Reinfusing chyme stretches the luminal walls of the bowel, which may cause abdominal discomfort. To reduce this discomfort, begin chyme reinfusion slowly. For more information, refer to the ETD-14 Patient Management listed on The Insides Company Training Portal.
a. While holding the pump against the driver, press the 'MODE' button to start at 'MODE 1', the slowest speed setting. If chyme moves quickly up the tube, stay on 'MODE 1' and reinfuse a small volume of chyme.
b. After 30 seconds, if chyme is not progressing up the
tube, increase to the next ‘MODE’. Continue this process until chyme is progressing up the tube. If chyme is not progressing up the tube after 60 seconds on 'MODE 5', refer to the Troubleshooting section below.
c. If chyme starts to reflux out of the stoma, or if the patient feels nauseous or bloated, reduce the 'MODE' on the driver or cease reinfusing for several minutes. Reducing the ‘MODE’ can be accomplished by pressing the ‘MODE’ button, which transitions through all five speeds and off. For further information about reflux, refer to the Troubleshooting section.
4. After reinfusing a small amount of chyme, decouple the driver from the pump and turn it off by cycling through each ‘MODE’.
Ensure the patient receives routine ostomy appliance changes. Make sure the patient takes care when removing the appliance so that the tube is not pulled out. The pump may get caught in the ostomy appliance upon removal. Ensure the patient holds onto the tube with one hand and removes the ostomy appliance with the other hand. If this is too difficult, detach the pump from the tube within the ostomy appliance to be removed together.
The time required to reinfuse chyme varies depending on the chyme's thickness, which may differ across the day and the patient's oral intake. THE INSIDES® System is not suitable for thick or fibrous chyme, therefore some chyme may be discarded. Any amount of chyme that is refed is beneficial.
The patients using THE INSIDES® System should adhere to the following steps for optimal results:
If reinfusion takes longer than expected or if the patient is unable to reinfuse, attempt the following remedial steps:
If none of these solutions work, THE INSIDES® System may not be suitable for the patient.
When using THE INSIDES® System, patients may experience reflux of chyme from the distal intestine, around the tube, back into the ostomy appliance. Reflux occurs when the distal intestine receives more chyme than it can accommodate. While reflux is not harmful to the patient, it can increase its time to reinfuse successfully.
Reflux may be reduced by:
NOTE: Loperamide and similar anti-motility therapies can cause constipation, blocking the intestine and preventing chyme reinfusing. Adjust the dose of motility therapies as required and refer to ETD-14 Patient Management with The Insides System if further action is needed.
As stated in the warnings, there is a low risk that THE INSIDES® Tube may migrate into the intestine, most commonly due to natural peristalsis or patient movement. Management of ube migration must only be performed by trained healthcare professionals.
The Tube Migration Management resource is available on our website and through The Insides Company Training Portal. This document provides detailed guidance on safe removal intervention procedures.
Patients must not attempt to remove the tube themselves under any circumstances. If migration is suspected, the patient should contact their healthcare professional immediately.
Any serious incident that has occurred in relation to THE INSIDES® System should be reported to the manufacturer and the Competent Authority of the Member State in which the user and/or patient is established.
If you would like to watch the Insides System setup video, watch the video below:
If you would like to watch a particular section of The Insides System setup video, choose the section below and watch the video:
The Insides Driver Feature Explanation
Performing refeeding for the first time
*Please note that some videos have been marked restricted and may require Youtube account login in order to access the video.
This work instruction is to act as a visual prompt and reminder of the key tasks but does not contain all the necessary information.
Before using this document, thoroughly read The Insides® System Setup Guide and The Insides® System Instructions and Technical Description.
a. Prepare The Insides® Tube

b. Unwrap the arms of retention sleeve.

c. Ensure the retention sleeve is positioned towards the base of the tube.

d. Ensure the guidewire sits in the tip of the bulbous feature.

e. Lubricate the bulbous section of the Tube.

1. Digitally palpate the distal intestine to determine if the Tube is suitable, and the direction and distance to the fascia

2. Prepare the Tube for insertion. Collapse the bulbous feature of the Tube by inserting the guidewire until the base of the Tube touches the stop of the guidewire. Pinch the guidewire through the tube to maintain the position.

3. Pinch the bulbous feature and roll it between your fingers to further collapse the Tube. Apply more lubricant if required.
ENSURE THAT THE GUIDEWIRE REMAINS WITHIN THE TIP

4. Hold the Tube and guidewire together firmly. Insert the Tube and apply gentle pressure until the whole Tube, up to the retention sleeve, is inserted into the stoma/fistula. This ensures the bulbous feature is beyond the fascia. The Tube can be inserted at any angle that is required.

5. Hold the retention sleeve to keep the Tube in place and remove the guidewire.

6. Allow the Tube to settle in its natural position then move the retention sleeve so it sits 1-2 mm away from the stoma.

7. Wrap the arms of the retention sleeve back in place.

8. Hold the ostomy appliance against the Tube and Pump to determine the appropriate length of tube.

9. Trim the Tube to the desired length.
10.Connect the Pump to the Tube. The Pump should be pressed up to the third ring.

11.Supervise the patient threading on their ostomy appliance and securing it to their abdomen. Ensure there is a 10-20mm gap between the Pump and the outlet.

12. Secure the Clip to the Tube when the patient stands up.

Before using this document, thoroughly read The Insides® System Setup Guide and The Insides® System Instructions and Technical Description.
This work instruction is to act as a visual prompt and reminder of the key tasks but does not contain all the necessary information.



This document is to be used in conjunction with IFU-1 The Insides® System Instructions and Technical Description, and IFU-2 The Insides® System Setup Guide for Healthcare Professionals
Before using this document, thoroughly read Gastrostomy Tube Insertion and The Insides® System Instructions and Technical Description.
This work instruction is to act as a visual prompt and reminder of the key tasks, but does not contain all the necessary information.
1. Prepare the workstation.

Prepare the Cook Entuit 24Fr tube.

Double bung the Enteral meds only port and remove the cardboard tag

Inflate the balloon with 10mL sterile water to ensure the balloon is symmetrical. Then deflate the balloon

Lubricate the tip of the Cook Entuit 24Fr tube
2. Digitally palpate the distal limb of the enterostomy or enteroatmospheric fistula. This is to gauge any narrowing, direction, and distance to fascia.

3. Insert the Cook Entuit 24Fr tube into the distal limb of the intestinal tract.

Slowly insert the tube with the dominant hand.

Guide the tube further into the stoma with the non-dominant hand to the predetermined length.

Move the cuff so it sits 1-2 mm from the Stoma outlet.
4. Inflate the Cook Entuit 24Fr balloon with 4ml of sterile water.

5. Thread the baseplate over the tube and adhere it to the skin around the stoma.

6. Connect the Insides Pump to the FEED ONLY port of the Cook Tube. The tube should be pressed up to the second ring of the pump

7. Place the tube in the Ostomy appliance and connect the bag to the baseplate.

Patients with an enteroatmospheric fistula or high-output enterostomy should be closely monitored when first introduced to The Insides® System. The following points should act as a guideline to ensure successful patient outcomes. This document should be used in conjunction with The Insides® System Instructions and Technical Description and The Insides® System Setup Guide.
Refer to The Insides® System Setup Guide for setup instructions to The Insides® System.
The first week of chyme reinfusion therapy for the patient is going to be the hardest due to the discomfort of reintroducing chyme into the distal intestine, learning how to change their ostomy appliance with the Tube in situ, troubleshooting, and minor modifications to their diet. Please establish this at the beginning and continue to provide support in the initial phase of chyme reinfusion therapy. In turn, please reassure the patient that this will pass and performing chyme reinfusion therapy will provide them with many benefits.
To provide further securement of The Insides® Tube (Tube), secure The Insides® Clip (Clip) to the outside of the ostomy appliance, over the Tube, and as close to the bottom of retention sleeve as possible. This Clip provides a second anchor point for Tube to stop it from sliding out from peristalsis. Please view How to use The Insides® Clip and Retention sleeve video and Patient applying The Insides® Clip video for further clarification.
During the first session, use the patient's chyme to demonstrate refeeding. Refeeding with chyme provides a more realistic understanding of the time requirement, which is longer than refeeding water. Chyme must be less than eight-hours old, and the ostomy appliance should be at least one-third full.
The patient's first refeed of chyme may cause lower abdominal discomfort and bloating due to bowel distension. A small volume of chyme should be initially refed, at regular intervals, to minimise discomfort.
The volume of refed chyme will vary among patients. For example, a patient with a newly formed stoma may be able to refeed 100 mL of chyme once or twice a day, while a patient who has been defunctioned for over a year may only be able to refeed 50mL in a day. Most patients take one week to be rehabilitate their distal bowel and refeed at least 90% of their output. It is not unusual for some patients to take up to a month to establish routine refeeding, and this is due to the increased length of time that the patient has been defunctioned. Increasing a patients tolerance to refeeding is explained further below. Mild to moderate analgesia can reduce patient discomfort if required.
For efficient refeeding, the patient should sit on the edge of the bed with their feet flat on the ground or standing up with at least three points of contact for balance. This ensures all chyme is sitting at the bottom of the ostomy appliance. Ensure the Tube is straight down in the ostomy appliance so The Insides® Driver (Driver) does not have to work against bends in the Tube. Ensure the patient has a good view of the Tube and can see the chyme moving up the Tube. Support them with finding a comfortable position to hold the Driver for effective refeeding.
The Tube can take up to 48-hours to settle into its natural resting position. Peristalsis may push the Tube out slightly, changing the resting position. The retention sleeve may need to be adjusted to ensure the Tube maintains a flat profile against the body. The Tube length may require additional adjustment to ensure that The Insides® Pump (Pump) is appropriately placed and not pressed against the end of the ostomy appliance.
The use of the Clip is helpful in this initial period to help keep the Tube in place and reduce movement.
The patient should feel comfortable while the Tube is in situ. Pain around the distal stoma, or significantly more Tube visible in the ostomy appliance, may signify that the Tube has slipped from underneath the fascia and is resting at skin level. If this occurs, the Tube will need to be removed and reinserted.
The patient should continue to refeed at very low volumes for the first few days and only increase to their own tolerance. This reduces the amount of discomfort they may get from bolusing chyme into a defunctioned intestine. Bolusing chyme stretches the luminal wall of the intestine which creates the discomfort. Please see the Frequently Asked Question: Increasing Patient Tolerance to Chyme Reinfusion for guidance on how to complete this safely. In the first week the patient may experience reflux which is chyme that has been refed but trickles back into the ostomy appliance. Reflux is not harmful but it does increase the length of time to refeed. Reflux occurs because the intestine is unable to absorb the volume of chyme that is being bolused. To reduce reflux, refeed little volumes, around 50 ml, every 2-3 minutes to assist in rehabilitating the distal intestine. Gently hold the retention sleeve on the Tube, up close to the mucosa of the stoma while reinfusing to encourage the bolus of chyme to be absorbed and reduce reflux.
When a patient refeeds using The Insides® System (System), chyme passes through the entire gastrointestinal tract; therefore, a patient's output is calculated as follows:
Output = Volume of Vomitus + Volume of Urine + Volume of Chyme Discarded into the Toilet
The output calculation does not include the volume of chyme, which is refed. Instruct the patient on maintaining the Patient Fluid Balance Chart, which will provide the healthcare team with an overall picture of device use and an accurate measure of the patient's fluid balance. Once the patient is home, encourage the patient to continue monitoring their fluid balance by using The Insides Log Book, that is provided in the System box. This will provide the healthcare team visibility on the patients progress while at home.
Once a patient has started refeeding, they can begin consuming food to wean off parenteral nutrition. Patients should start oral feeding slowly with small meals and it is recommended to be under the guidance of a Dietician. Once a patient starts oral feeding, their output will increase, please reassure the patient this is expected and will slow down once their distal bowel is rehabilitated and adjusting their anti-motility medication. Patients should chew their food well and avoid stringy, fibrous foods to ensure that the Pump does not block. Refer to the Dietary Recommendations for The Insides® System for more information.
Refeeding with The Insides® System provides a longer length of bowel for absorption. Medication toxicity is possible for patients on oral medications with a narrow therapeutic range, such as Warfarin. Closely monitor drug levels and adjust doses, where necessary, when using The Insides® System.
If the patient is using a night bag to collect night time losses to reinfuse in the morning (within eight (8) hours), short-acting-medication must be taken four (4) hours before attaching the night bag. This is to ensure the medication has transited and been reinfused down stream before attaching the night bag.
Monitor drug doses closely during the initial phases of refeeding and when the patient is discharged home as compliance is likely to drop.
Close monitoring of biochemistry, renal blood levels, increasing oral feeding, and reducing the amount of chyme discarded will guide weaning off PN and IV fluids. Refer to the Suggested Chyme Reinfusion and Parenteral Nutrition Weaning Guidelines for more information. Time taken to wean off PN will be dependent on individual patient characteristics but ensuring a level of independence with the device is necessary so that patients are able to maintain high use of the device.
Patients will likely have a bowel movement within the first two to four days of refeeding, depending on the frequency and volume of refeeding. The frequency of bowel movements is also influenced by the patient's physiology and the amount of colon that remains intact. The first bowel movement will likely have a Bristol 5 or 6 consistency, progressing towards a Bristol 3 to 4 by the end of the second week. Bowel movement consistency will be affected by Loperamide use and length of colon the patient has available for reabsorption.
Reintroducing chyme downstream may ignite a Clostridium difficile infection that was lying dormant in the colon. If this occurs, monitor the patient and treat it accordingly. Low-level colitis may be present in patients that have been defunctioned for an extended period. This complication should resolve in 2-3 weeks.
Consistently encourage and support the patient to use The Insides® System independently throughout the first week. This includes modifying their process when changing their ostomy appliance. Support and monitor the patient the first few times they change their ostomy appliance so they understand how to safely thread the ostomy appliance over and off the Tube and Pump and then when resecuring the appliance once the Pump has been changed. Allow the patient to practise and record their use to improve their understanding and refeed as part of their daily routine. A well-supported patient in the hospital will likely continue to use the device once at home.
Patients may be ready for discharge to home in the second week. Before discharge, ensure that the patient's blood results are trending towards normal. If the healthcare team is satisfied with the patient's progress and is adequately competent with The Insides® System, they may be discharged home. Refer to Discharge Planning Checklist to ensure a safe discharge home. Utilise the Community Referral form to assit with a smooth transition home.
A stomal therapist trained on The Insides® System should visit the patient within 48-hours after discharge. The goal of the home visit is to address and troubleshoot any issues with the System.
Once discharged home, the patient may become dehydrated, leading to acute renal impairment. This issue occurs most often when:
To address issues with dehydration and renal impairment:
The following device use and patient monitoring assessments should be conducted once the patient is discharged:
At this stage, the patient will be returning to their regular routines, including returning to work, resuming household duties, and reducing visits with the stomal therapist. Compliance with the System may wain, and renal impairment may increase during this period. Regular creatinine/eGFR monitoring is crucial during this stage to negate renal impairment.
Proper use of The Insides® System and adequate nutrition will prepare the patient for a successful stoma reversal surgery. Increasing protein and carbohydrate stores with positive weight gain optimises recovery.
Once the patient becomes independent with The Insides® System, visits from the stomal therapist will decrease. The stomal therapist will still need to visit once a month to change The Insides® Tube and conduct assessments. Regular weekly phone calls with the patient renal monitoring will continue where clinically indicated.
Discharge Planning Checklist
Patient independence
Is the patient independent with using The Insides® System and simple trouble shooting?
Is the patient independent with their ostomy care in relation to Tube and Pump management?
Has the patient been given advice on signs and symptoms of dehydration and other complications that require them to return to hospital? (Return advice)
Medication
Has their medication been reviewed and reconciled by the Pharmacist to account for potentially higher enteral absorption?
Community Stomal Therapy Team
Have the receiving stomal therapy team received training on The Insides® System and patient management?
Does the stomal therapy team know how to order Refill kits?
Is there wound care follow up required?
Ensure contact details for clinical support with The Insides Company have been provided.
Patient information and supply
Has a surgical team follow-up plan been arranged for the patient?
Does the patient have the contact details for their local stomal therapy nurse?
Does the patient have the Patient Guide to Chyme Reinfusion Therapy with The Insides System
Do they have a lab form for bloods once discharged home?
Does the patient have enough ostomy supplies and Pumps for the first two weeks at home?
Is the patient able to access/pick up their discharge medication?
The Insides Driver is unable to handle thick viscosities of chyme. Please refer to The Insides® System Instructions for Use and Patient Management sections in the training hub.
As a general guide, an output over 1 Litre/24 hr should be thin enough to reinfuse. If the patient’s chyme is consistently too thick, measures will need to be taken to thin the chyme. This may include:
• Reducing anti-motility medication
• Drinking one to two extra glasses of water
• Drinking one to two cups of coffee
Please refer to the Patient Management section in the training hub.
Reflux is not harmful to the patient but it does increase the length of time taken to reinfuse their chyme.
Reflux could happen:
• High speed – A thin viscosity chyme, reinfused at a high setting on The Insides Driver will cause reflux and increase the time taken to reinfuse. The Insides Driver should be set at the lowest speed that moves the chyme through The Insides Tube.
• Constipation – The patient may be constipated from high dose anti-motility medication. The anti-motility medication needs to be weaned to reduce this. The distal bowel needs to be cleared for effective chyme reinfusion to occur.
• Atrophied distal bowel – The distal gut needs to be rehabilitated slowly. The patient will experience more reflux in the beginning because the luminal walls need to expand and rehabilitate. Small boluses regularly throughout the day will achieve this and reduce the reflux.
Please refer to the Dietary Guidelines pamphlet in the training hub. The dietary information pertains to use of The Insides System, it does not provide general patient dietary information.
Thin ‘stringy’ fibrous food gets caught in the back of The Insides Pump which reduces effective pumping. Avoid or blend fibrous food to ensure more effective chyme reinfusion.
Please refer to The Insides® System Instructions for Use and Patient Management sections in the training hub.
Rehabilitating an atrophied distal gut and initiating chyme reinfusion stretches the luminal walls of the intestine. This stretch can generate a diffuse abdominal discomfort, nausea, and bloated feeling for the patient. The longer they have been defunctioned, the increased level of atrophy and subsequent symptoms the patient will experience. Following the provided guideline on increasing tolerance will reduce the symptoms for the patient, ensure patient compliance, and rehabilitate the patient’s gut within one to three weeks. Once the gut has been rehabilitated, these symptoms should resolve.
While the patient is increasing their tolerance to chyme reinfusion, there will be chyme discarded directly from the ostomy appliance. These net losses can be recorded on the Patient refeeding record. As the distal gut rehabilitates, there will be reduced net losses and more bolus chyme reinfusion. Once the distal gut has been rehabilitated, the patient should be reinfusing as much of their output as they can.
The Insides Driver does not have a flow rate because chyme is made up of fluid and particles. Very thin/water like chyme will be reinfused quicker in comparison to thicker chyme. Thicker chyme will take longer because the Pump complex needs to grind the particles to generate enough pressure to move it up the Tube. It is best to chew food well so there is less work for the Pump. Use the lowest speed that moves chyme up the Tube to reduce patient discomfort and reflux. An ostomy appliance holds 200-300ml of chyme, this can usually be pumped through in under 5 minutes.
A trained healthcare professional must always insert The Insides Tube. The Insides Tube gets replaced every 28 days.
The patient changes The Insides Pump every two to three days along with their usual ostomy appliance change.
Yes, you can for the hydration benefits. However, the proximal outlet must originate in the small bowel, so chyme is the right viscosity to reinfuse. It is best if the distal colonic outlet originates from the ascending colon to maximise the hydration benefits and reduce the incidence of loose stool being passed rectally. Please refer to the The Insides® System Instructions for Use on tube insertion.
A common side effect of chyme reinfusion is the discomfort, nausea, and bloating felt in the first week. This soon resolves once the gut is rehabilitated.
The bowel length, that is external to the fascia, can be kinked and lengthened with a parastomal hernia. Caution is required when intubating a patient with a parastomal hernia. Digital palpation is required to gauge length, kinking or narrowing and direction to safely intubate the distal limb of the enterostomy. If there is any resistance or pain for the patient, they are unsuitable for chyme reinfusion. If digital palpation does not identify any concerning features of the hernia, then careful intubation by a trained health care professional is recommended. It is recommended that a balloon retained tube be used rather than The Insides® Tube in this instance.
• Ask a family member/carer to assist the patient with reinfusing their chyme.
• Swivel the pump around, so the flat surface is facing the back of the ostomy appliance. Then rest The Insides Driver up-side-down on their lap and couple The Insides Pump on top. Ensure the front panel of The Insides Driver can be seen by the patient or carer. Position the ostomy appliance so that gravity keeps the chyme sitting on top of The Insides Pump. Get the patient or carer to press the chyme onto The Insides Pump if necessary.
Most patients hold The Insides Driver with their dominant hand, with the front panel facing up so they can see it and are able to press the “Mode” button to move through the speeds. Their non-dominant hand holds the back of the ostomy appliance, “cupping” the chyme and pressing it into the back of The Insides Pump. When “cupping” the chyme, ensure the patient uses the flat of their hand to press into the back of The Insides Pump so there is no risk of cutting or crushing of fingers from the macerator within The Insides Pump. Use gravity to assist with keeping The Insides Pump submerged in the chyme. Encourage your patient to find a position that is comfortable and efficient for them.
The Insides Pump should intuitively fit into the hold at the back of the Insides Driver. The Insides Driver and The Insides Pump should be coupled first, before pressing the ‘Mode’ button to initiate chyme reinfusion.
• Blocked Pump – Try the following Troubleshooting Tips to unblock The Insides Pump otherwise, change The Insides Pump. To stop The Insides Pump from blocking, stop eating stringy fibrous food which blocks The Insides Pump.
• The Insides® Pump – Ensure The Insides Pump is fully submerged in the chyme.
• The Insides® Driver – Ensure all speeds on The Insides Driver have been tried for a minimum of 30 seconds each, to ‘pump’ the chyme up The Insides Tube. Sometimes the thicker chyme viscosity’s move slowly up The Insides Tube.
• Not coupled correctly – Ensure the flat surface of The Insides Pump has been cleared of debris and intuitively couple The Insides Driver with The Insides Pump through the ostomy appliance. Carefully hold The Insides Driver up and The Insides Pump should remain coupled. This demonstrates they are coupled effectively.
• The Insides Driver bounces off The Insides® Pump – This can happen at speed 5 or if The Insides Pump is blocked.
• Tube not anchored below the fascia – The bulbous anchor may have slipped underneath the fascia. The patient may be in discomfort or you will see an increased length of tube in the ostomy appliance that could indicate it has slipped out. If The Insides Tube is not intubated correctly, there will not be effective chyme reinfusion.
• Chyme is water thin, I have tried everything, but it is still not pumping – This may happen with a balloon retained tube. A bubble of air may be trapped within the tube, creating an airlock. ‘Milk’ the tube by pinching and folding the tube to break the air bubble. This may need to be done several times. Manipulate the tube in and out about 1cm to ensure free movement of the tube.
• Stool on the tip of the tube – If The Insides Tube or balloon retained tube is showing an increased length of tube in the ostomy appliance and it is not painful for the patient, but chyme is not transiting though the tube, there could be stool coating the tip of the tube. See images below. This may happen due to the patient not having effective bowel preparation before surgery or high levels of anti-motility medication. Inserting a new tube is recommended.
If the patient has an enterocutaneous fistula (ECF), please consult with The Insides Company’s stomal therapist for an individualised solution.
It is known that pouching a patient with an ECF can be extremely difficult and distressing for the patient. It requires trial and error with many products and techniques in order to protect the peri-fistula skin and direct the flow of chyme into the ostomy appliance.
Things to consider:
• Reflux – A constant flow of chyme over the hydrocolloid at the aperture of the ostomy appliance will degrade the hydrocolloid quickly and cause leaks. Review the cause of reflux.
o Reduce the speed of the Insides® Driver to reduce reflux.
o Reinfuse smaller and more frequent boluses to reduce reflux.
o Is it temporary and will resolve once the gut has rehabilitated?
o Is the patient constipated?
Due to the undulating abdominal landscape, accessories such as hydrocolloid seals and paste are strongly recommended. Consider building up the seals to increase absorbency and reduce the deterioration of the seal.
• Chyme viscosity – Water thin chyme not only increases the risk of dehydration but also the risk of the chyme sliding underneath the aperture of the ostomy appliance and creating a leak. Consider thickening the chyme via anti-motility medication to reduce this risk. However, the thickness of chyme must remain within a normal range to reinfuse. Anti-motility drugs can also cause constipation downstream of the stoma.
• Retention sleeve – Does the retention sleeve on the Tube get caught on the aperture of the ostomy appliance? Lift the tube into a horizontal position when threading the ostomy appliance on. This ensures the retention sleeve clears the edge of the ostomy appliance and sits completely inside the pouch.
• Night bag – To stop chyme pooling at the aperture of the ostomy appliance, attach a night bag to the end of a high output drainable ostomy appliance. This creates a vacuum and draws the chyme away from the aperture. If this option is used, ensure the patient is wearing a 2 piece or an ostomy appliance with a window so chyme can be transferred back into the pouch to be reinfused.
• Ostomy appliance – Ensure all recommended manufacturer’s guidelines are being followed when applying the ostomy appliance. An example of this is warming the hydrocolloid before application.
Caution is required when testing the function of a patient’s J pouch or ileal pouch-anal anastomosis (IPAA). The patient needs to be made aware of the effect of bolusing chyme into a J pouch. Reinfuse a small amount of chyme at a low speed.
The patient needs to be reviewed by their surgical team as to the cause of the issue.
Yes, but you must complete the following steps to do it safely. Please refer to the Patient Management section in the training hub.
• Reinfuse all chyme sitting in the ostomy appliance immediately before attaching the night bag.
• Take any short-acting medication at least four (4) hours before attaching the night bag. This ensures the medication has been digested and reinfused before the night bag has been attached so there is negligible medication sitting in the night bag.
• Chyme sitting in the night bag must be reinfused within twelve (12) hours. For example, if the patient attaches the night bag at 10pm they must reinfuse what is sitting in the night bag between 9am – 10am the next day. If chyme sits in the ostomy appliance for longer than twelve (12) hours, it should be discarded.
Yes, please refer to the Suggested Chyme Reinfusion and Parenteral Nutrition Weaning Guidelines document.
No, nothing should be added to a patient’s ostomy appliance to reinfuse. Only intestinal content that naturally passes into the patient’s ostomy appliance should be reinfused except for water during the initial testing.
• Please advise the patient that rehabilitating their distal bowel will likely be an uncomfortable experience, but it will be managed slowly, and discomfort kept to a minimum. Please reassure your patient that the discomfort will pass once their bowel is rehabilitated.
• Please refer to Please refer to The Insides® System Instructions for Use and Patient Management sections in the training hub. Reinfuse 50ml of chyme once daily and very slowly increase the frequency to their tolerance. This may take up to three (3) weeks.
o If chyme starts moving up the Tube on speeds 1 – 3, approximately 50 ml would be reinfused in 15 seconds.
o If chyme starts moving up the Tube on speeds 3 – 5, approximately 50 ml would be reinfused in 30 seconds.
• It is recommended to start with The Insides Tube 22 Fr for the first 28 days before moving onto The Insides Tube 28 Fr.
• Do not start weaning off anti-motility medication and having large meals until the patient is sufficiently rehabilitated. This is to mitigate increased output into the ostomy appliance and increasing the risk of dehydration.
Yes, you can but please consider the following:
• The output that is being reinfused must be chyme, originating from the small bowel so the viscosity will work with The Insides System.
• What is the goal?
o For preservation of the out of circuit intestine that will not be resected at the time of reversal?
o Maximising nutrition?
o Maximising hydration, or both?
• Does the patient have the dexterity, enthusiasm, and family/friend support to manage two tubes, and thus two bolus reinfusions?
• Guidance around manging two (or more) reinfusions systems:
o Focus should be placed on reinfusing the most proximal distal limb to ensure maximal absorption of nutrients.
o Introduce the second reinfusion once the patient is confident with the first. This must be a slow methodical titration to ensure the patient is coping.
o Provide support around ostomy appliance changes until they are independent and confident
o If the second double barrel/fistula outlet (distal to the first) is located in the distal jejunum/proximal ileum, reinfuse as often as possible into this distal limb as well.
o If the second double barrel/fistula outlet (distal to the first) is located in the distal ileum/ascending colon, reinfuse chyme into this distal limb as much as clinically indicated to ensure nourished and hydrated (This may mean onl7 2-4 times per day)
o Once the terminal ileum is back “in circuit”, a patient’s output will thicken up considerably so ensure the patient knows how to thin their output, wean off anti-motility medication and perhaps reduce reinfusions to twice a day (discarding thick output that cannot be reinfused).
• Follow up with the patient regularly to ensure they are managing well. Pause reinfusing the second distal outlet if there are concerns around coping and restart once the patient is ready.
• Regularly reassess the goals of reinfusion.
Please refer to the Patient Management section in the training hub and this question, Can I use a night bag attachment to capture my night-time output?
Please refer to Prior to reinfusing with The Insides System on the training hub.
Please refer to Prior to reinfusing with The Insides System on the training hub.
Please refer to Patient Management on the training hub and this question - What do I do about reflux?
Antimotility medication can cause constipation downstream, causing more reflux. Clinically assess for constipation and adjust the dose of antimotility medication as required. Clinically assess requirement for aperients and contact The Insides Company Clinical team for administration guidance.
Unless advised by the surgical team, the patient can reinfuse their chyme to the day of surgery.
There are 2x 28 Fr tubes and 1x 22 Fr tube supplied.
These clips provide further securement of The Insides Tube. The Insides Clip is placed on the outside of the ostomy appliance, over the Tube (think of a clothes peg), and sits as close to the bottom of retention sleeve as possible. How to use The Insides Clip and Applying The Insides Clip video can be found on the training hub. The Clips are colour coded:
• Purple Clip can be used on the 28 Fr and the 22 Fr Tube and is placed on the widest part of the tube (this is 39 Fr), distal to the retention sleeve.
• Orange Clip is used with the 28 Fr tube and is placed on the 28 Fr portion of the tube if it is unable to be fully inserted into the intestinal outlet.
• Yellow Clip is used with the 22 Fr tube and is placed on the 22 Fr portion of the tube if it is unable to be fully inserted into the intestinal outlet.
There are 3x Insides Tubes provided in The Insides System to help mitigate any tubes falling it. It is expected that the tube will fall out at least once in the first week.
There are 3 possible reasons for this:
• The patient accidentally pulls it out when they change their ostomy appliance.
• Peristalsis is pushing the tube out. The Tube usually stays in for 1- 2 days and then spontaneously slides out. Encourage the patient to hold Tube retention sleeve when reinfusing and walking around. After the first week, this should stop because true peristalsis has been re-established. The Insides Clip will assist with this.
• The surgical cut in the fascial layer, where the proximal and distal end is brought through, is too wide to retain the bulbous feature of Tube, so it just slides out. The Insides Clip will assist with anchoring it in place. However, please talk with The Insides Company Clinical team if this continues.
• If the Insides tubes keep falling out, we suggest trying a balloon retained feeding tube.
• If all other resolutions fail, another option to keep the Insides tube in situ is to use a second convex ostomy appliance, placed back to front, directly over the primary ostomy appliance that is secured with an stoma belt. Placing an entire ostomy appliance over removes pressure points and offers a wide surface as a “back-stop” to keeping the Tube in place. An example:
Drivers are Single Patient Use only and must not be used with more than one patient for regulatory, and health and safety reasons. Please dispose of The Insides Driver upon the reversal of the patients enterostomy or fistula according to the local disposal authority. Please refer to The Insides System - Instructions and Technical Description contained in the packaging for further guidance.
Do you have any suggestions on what ostomy appliances and accessories that work best with the device?
We recommend using the ostomy appliance and accessories that work best for the patient. The Insides System fits within the patients preferred appliance. However, if the patient has reduced dexterity, it may be easier for them to use a 2-piece ostomy appliance. Please refer to Prior to reinfusing with The Insides System on the training hub for further guidance.
No, we have not receieved any feedback from customers regarding this. We do strongly recommend clinicians read and understand The Insides System - Instructions for Use and the documents contained on the training hub prior to starting the device with their patient.
It is very unlikely the ostomy appliance however, if this occurs, please contact The Insides Company Clinical team to resolve.
What is the concern directly relating to?
• Having a tube in situ consistently with concern around being able to undertake activities of daily living?
The only way to know for certain is to place the Tube and monitor and support the patient to work with this. Slight modifications to bodily movements may need to occur. For example, bending over to tie a shoelace; the patient may need to place their foot up on a bench to tie the shoe lace.
• Access to the distal outlet is narrow
Digital palpation is recommended first. If the smallest finger is unable to be inserted downstream, it is likely a 20 Fr balloon retained feeding tube will be required. The next time the tube is changed, do assess to see if rehabilitation of the distal limb has increased the calibre of the outlet so the Insides 22 Fr Tube is now able to fit.
• There is a kink (that does not have an Inflammatory Bowel Disease aetiology) in the intestine, close to the distal outlet, that may not be able to be navigated around with the tube.
Cautious clinical assessment is required, if safe to proceed, there are two options:
Place a smaller bore tube downstream that can navigate around the kink. Keep this in situ for several days and manually reinfuse saline to assist with increasing the calibre of the distal limb. Attempt a larger bore Tube after this time.
Endoscopically place the Insides tube or balloon retained tube that is 20 Fr or larger and keep in situ for 28 days. The tube will likely ‘straighten’ this portion of intestine so bed side installation of the Tube is achievable next time.
The continuous enteral feed was trickling into the distal limb at a consistent rate which simulates normal peristaltic movements and doesn’t stretch the luminal walls like a bolus administration of chyme with the Insides Driver does. There will be a period of adjustment for the distal intestine to become accustomed to a bolus of chyme but this will likely resolve within the first week due to the prehabilitation from continuous enteral feed. If there is still pain or discomfort after 2 weeks, assess and find cause. There maybe be an unidentified obstruction/narrowing/stenosis that spontaneously occurred. Previous surgery that resulted in an anastomotic join distally may have contracted during healing that is causing pain or discomfort that was not previously identified due to the administration switching from continuous to bolus.
The Insides System has not been tested above that height, so it is not indicated to be used above 3000m.
There is a safety mechanism in place that if The Insides Driver runs completely flat it will not recharge on a single charge. We recommend the Driver is charged for two (2) hours every week to ensure it doesn’t run out of battery. If the Driver runs flat:
1. First ensure you are using the correct wall charger. The Driver only charges with its own charger
2. Connect it to the wall charger and wait for approximately 15 minutes for the lightning bolt to flash on the front panel.
3. Disconnect it, wait 1 minute and reconnect to the wall charger.
4. Repeat step 1 and 2 several times until the Driver can hold a charge and completes a full charge.
5. If this does not charge the Driver, please contact your local distributor or The Insides Company.
Please present this information to the patients Cardiologist to evaluate if they are eligible:
The device passes the EMI standard for a medical electrical device IEC60601-1-2. But it also has strong rotating permanent magnets (rotate from 0-5000 rpm). These permanent magnets are not specifically evaluated under this standard.
To complete this competency framework and be deemed competent, a nurse must undertake the following:
Upon completion on the framework, a nurse will be competent in the following skills:




All copyright, design and intellectual property rights existing in our designs and products and in the images text and design of our website are the property of The Insides® Company. The innovations developed by The Insides® Company are covered in one or more pending patents.
The following are pending patents of The Insides® Company:
WO2019073365(A1)
WO2019171335(A1)
WO2022224175A1
The following are registered patents of The Insides® Company:
CN111818885B
AU2018349270B2
The following are registered designs of The Insides® Company:
CN307984577S
30202300143W
30202300144U
AU202217736
AU202217737
EP015007939-0001
EP015007939-0002
UK6253298
UK6253299
NZ430941
NZ430942
The following are trademarks of The Insides® Company:
The Insides
The Insides Company

Please contact the company for an updated list of IP.
‘Coloplast’, ‘SenSura® Mio ’ are registered trademarks of Coloplast Corporation. The use of the trademarks ‘Coloplast’, ‘SenSura® Mio ‘in these instructions is strictly for informational purposes to provide accurate product information to our customers. The Insides Company Limited does not connote any endorsement, affiliation, sponsorship, or approval by Coloplast Corporation. We hereby affirm our recognition of Coloplast Corporation 's exclusive intellectual property rights in the trademark ‘Coloplast’, ‘SenSura® Mio,' and any references to said trademark are made in good faith to truthfully describe the compatibility or usage of their product.
‘Hollister’, ‘Pouchkins™’ are registered trademarks of Hollister Incorporated. The use of the trademarks ‘Hollister’, ‘Pouchkins™‘in these instructions is strictly for informational purposes to provide accurate product information to our customers. The Insides Company Limited does not connote any endorsement, affiliation, sponsorship, or approval by Hollister Incorporated. We hereby affirm our recognition of Hollister Incorporated 's exclusive intellectual property rights in the trademark ‘Hollister’, ‘Pouchkins™,' and any references to said trademark are made in good faith to truthfully describe the compatibility or usage of their product.