
Left to right:Katy, Mary*, George*, Jane* and Becky
*Aliases used to protect privacy
Written by:Katy Martin-Skurr CNS Stomal Therapy
The following two case studies describe how critical thinking and stomal therapy skills were challenged during the management of two patients with complex enterocutaneous fistula (ECF).
Enterocutaneous fistulas are abnormal connections between the gastrointestinal tract and the skin that appear spontaneously or following surgery. Dehydration, electrolyte imbalance, malnutrition, renal impairment, intestinal failure, and sepsis are complications associated with ECFs. These complications result in substantial morbidity and mortality with increased hospital stay and a high financial cost (Bhat et al., 2020).
A high volume of intestinal output, and peri-fistula skin problems can make management of these patients challenging for the multidisciplinary teams (MDT), which includes the stomal therapist (STN). Having an ECF impacts on the patient’s quality-of-life and has psychological effects for patients and their family or whānau (Brook et al, 2019). Patient engagement and family or whānau support are also important for successful management and improved quality-of-life. A holistic collaborative approach is imperative for successful treatment resulting in more positive patient outcomes.
Patients with an ECF have a long journey to recovery. Careful timing of surgical repair is essential to minimise further complications and ensure patient safety and successful outcomes. At least six months is required before surgical repair of the fistula should be attempted, to ensure adhesions have softened and the tissue is in a workable state (Bharma, 2019).
The two case studies outline the collaborative approach to care, that includes guidance from the National Intestinal Failure team, utilising chyme reinfusion therapy administered via The Insides® System (The Insides® Company, Auckland, New Zealand).
George* is a 73-year-old retired New Zealand European gentleman who lives with his wife Jane*. He has a supportive extended family living locally. He has an extensive medical history of ischaemic heart disease, hypertension, and atrial fibrillation. His journey began in 2016, with the following unfortunate complications:

Five years later, following complex management of chronic discharging wounds, George had the following surgery and complications:

Wound clinical nurse specialist (CNS) and stomal therapy referrals were made. The Stomal Therapy and Wound CNS visited the High Dependency Unit to assess George’s wound. With limited knowledge of the ECF and minimal supplies, the wound/fistula was managed as follows:
The following day, the effectiveness was evaluated. The ECF continued to drain dark brown watery chyme (<2000mls) and the nurses reported stoma appliance leakage. The stoma appliance was replaced adding the following:
Later, HyalO4 control spray was applied to the problematic area at the chyme leak point. HyalO4 contains hyaluronic acid sodium salt and metallic silver (Figure 5.). This prevents bacterial contamination and provides conditions for wound healing (Fidia Farmaceutici SPA, 2021).
The successful use of this system continued for two months.
The STNs attended to the stoma appliance change on most occasions with the assistance of the ward Registered Nurse (RN) or Wound CNS. The fistula/wound management plan and templates were updated weekly to ensure the ward team were educated and a consistent approach was implemented. To maintain a low biome wound bed between twice weekly pouch changes, a windowed Eakin Pouch was used to enable twice daily irrigations and manual suctioning. The procedure took 45-60 minutes.

A holistic collaborative approach was required with the management of George’s overall care including his surgeon, dietitian, pharmacist, physiotherapist, psychologist, nursing staff, wound CNS and STN. The STN took the lead nursing role to advocate for George, collaborate with the MDT, and support and educate the nursing staff.
The initial management of nutrition and electrolytes was achieved with total parenteral nutrition (TPN) and intravenous fluids via a peripherally inserted central catheter (PICC) line. A strict fluid balance was necessary and regular blood tests to monitor electrolytes, renal, liver function tests, full blood count, and C Reactive Protein (CRP). The dietitian notified the National Intestinal Failure team following 30 days of TPN, which continued for three months.
Loperamide was titrated up to 36mg/24 hours and Codeine Phosphate 60mg twice daily was administered to reduce gastric emptying by reducing peristalsis. Omeprazole was also given, and 24 hours of Octreotide was administered to dry up secretions. This targeted therapy resulted in reducing George’s output to 1000-1500mls/24 hours.
Regular analgesia that resulted in pain relief for George was achieved with BD Oxycontin and PRN doses of Oxynorm, 30 minutes prior to pouch changes.

Ten weeks later, a low residue, high protein, low calorie diet was commenced to optimise his condition in preparation for surgical repair. Introducing an oral diet resulted in thickening and reducing chyme volume, and TPN was able to be discontinued due to George meeting his nutritional needs orally. Oral fluid intake of two litres was encouraged which included Fortisip and oral electrolyte solution, Electral. Five sachets of Electral in one litre of water was advised daily. Minimising hypotonic fluids (e.g. free water, tea, coffee, juice) was also recommended and follows guidelines for the management of high output ileostomies as described by Stankiewics, et al. (2019).
At twelve weeks, in collaboration with the National Intestinal Failure team, it was decided to trial the use of the chyme reinfusion system, The Insides® System from The Insides® Company (Auckland, New Zealand). This therapy involved a gastrostomy tube being inserted distally. The Insides® Pump was attached to the tube and sat within the pouch, submerged in the chyme (Figure 6 & 7). The Insides® Driver would be coupled magnetically on the outside of the pouch to The Insides® Pump when there was adequate chyme. The Insides® Driver activated The Insides® Pump to drain chyme from the pouch, down the tube and into the distal bowel (Figure 7 & 8).
The benefit of chyme reinfusion is the restoration of distal gut function. It can reverse gut atrophy, inflammation, and improve the gut microbiome. It also improves nutrition by enabling early return to oral feeding and the reabsorption of important nutrients. Reinfusing chyme prevents dehydration therefore reducing risk of acute and chronic kidney injury. It is also said to reduce liver function abnormalities as TPN can be ceased (Picot et al., 2016). A 2019 study by Duan et al found that chyme reinfusion for patients with loop ileostomies and Crohn’s disease resulted in lower rates of post-operative ileus following reversal surgery. This could also be another potential benefit following surgical repair of ECF.

George managed the chyme reinfusion independently and was well enough to be discharged three weeks later after a trial long-weekend at home. The discharge plan was to attend the Stomal Therapy Clinic on Monday, Wednesday, and Friday for pouch change and monitoring, including for dehydration. Readmissions with dehydration account for 30% of readmission rates following colorectal surgery according to Chen et al., (2018), so reducing this risk for George was paramount.
The Gastrostomy tube was replaced by the STN monthly and The Insides® Pump was replaced at each pouch change. George also attended outpatient appointments every 1-3 weeks. Initially he had weekly blood tests to monitor renal function and electrolytes.

Mary* is a 56-year-old Māori woman who has supportive adult children and extended whānau/family living locally. She also has her 16-year-old grandson living with her. She was carrying extra weight, weighing 128kg and a BMI of 51, suffered from hypertension and has had a previous ovarian cystectomy. Her surgical journey proceeded as follows:


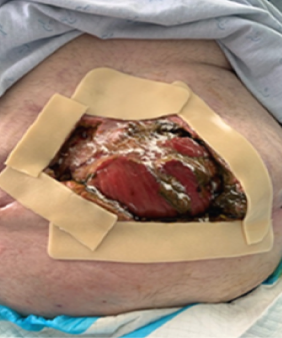
STN and Wound CNS attended to assess the wound and create a management plan. The wound was situated under her large abdominal apron, the lateral wound edges were held together with sutures leaving an open wound of 15cm (Figure 9). Unfortunately, the chyme discharge was leaking out between the sutures. After two weeks it was decided to remove both the drain and the sutures leaving a 26cm wound. Pouching was necessary to contain the chyme however, this was not an easy task due to the wound length and location. The principles to the management of her fistula were similar to George, but the location provided huge pouching challenges. After some failed attempts, lifting her abdomen using Hyperfix tape was trialled (Figure 10). This was transformative as it prevented the skin fold sandwiching, allowing improved drainage and provided a longer ostomy appliance-wear time. Initially a double pouching system was required using large Eakin wound ostomy appliances attached to one Atrium low pressure drainage system with a ‘Y’ connector. As the wound healed, we progressed to a single extra-large Eakin wound ostomy appliance (Figure 10 & 11).

The procedure required two nurses plus a nurse or Healthcare Assistant (HCA) to hold the abdominal apron.
The fistula output increased to 1500ml-2000ml so a collaborative team approach with the MDT including the surgical team, dietitian, physiotherapist, psychologist, wound CNS and STN was employed to manage this. Initially Mary’s nutrition was managed with TPN, IV fluids and nil by mouth. To reduce fistula output, Mary was treated with Loperamide and Codeine. Regular analgesia was important especially prior to pouch change.
Emotionally Mary blamed herself for the complications and wound care problems. She believed her obesity caused it to be more challenging. Reassurance, consistency of care and psychological input was an ongoing necessity.

After three months, The Insides® System was initiated, and a gastrostomy tube was inserted to start reinfusing Mary’s chyme (Figure 12). A low residue, high protein, low calorie diet was commenced and the TPN was discontinued soon after. Mary was independent with chyme reinfusing after three weeks and was discharged home. By starting chyme reinfusion, it was found that Mary’s output and subsequent leaks were reduced because chyme was drawn away (and reinfused) which stopped the pooling and ostomy appliance failures.
The discharge plan consisted of the following:

As the wound healed the pouching system evolved. Placing the Hyperfix binding first allowed for a two person procedure as it held the skin fold upwards. This enabled the wound to be cleaned and the ostomy appliance to be replaced more successfully.
Mary would take Loperamide half an hour prior to the procedure, this in most instances, allowing the process to be completed without continuous output.
The following products were used:

This pouching system was replaced three times per week.
The complex management of ECFs for these two patients was challenging and tested both critical thinking and creativity with all facets of care. Multiple ostomy and wound products were used to manage output and prevent skin breakdown. Nutritional support, oral electrolyte solution and chyme reinfusing systems enabled George and Mary to be discharged home while waiting on definitive surgery. The STN and wound CNS supported them alongside the psychologist and surgical team.
Whilst their journeys were not without problems, they both reported confidence in the team caring for them and the ability to be at home improved their quality of life significantly. George and Mary are currently awaiting their reversal surgeries at home, rehabilitating and optimising their recovery while enjoying the comforts of home.
Katy is not an employee of The Insides® Company and has not received any compensation for these case studies from The Insides® Company.
"I have worked within surgical specialties for 30 years with a particular interest in colorectal nursing. Prior to taking on the stomal therapy position, I was a preadmission CNS and surgical ward coordinator. With these positions, I was involved in the implementation of the Enhanced Recovery After Surgery (ERAS) program for both bowel resection and radical cystectomy patients. I heard that the stomal therapist was soon to be retiring and at that point, I decided that becoming a stomal therapist is what I wanted to do."
"I am passionate about evidenced based nursing and love the challenge that stomal therapy provides. I am currently completing post graduate study with the hope of becoming a nurse prescriber next year."
"I enjoy supporting patients throughout their journey and the problem solving that comes with it."
*Aliases used to protect privacy
Individual results may vary. Testimonials do not claim to represent typical results. All testimonials are received from real patients via text, in person, or through video submission, and may not reflect the typical patient experience. Testimonials are not intended to represent or guarantee that anyone will achieve the same or similar clinical results. Each patient’s condition is unique to their physiology and health status. Thus, the testimonials shared by The Insides Company may not reflect the typical patient experience.

This case study follows Jaybie, a preterm infant born with gastroschisis who required multiple abdominal surgeries and experienced a complex postoperative course. She developed intestinal failure, became dependent on intravenous nutrition, and faced a long and challenging path to discharge...

This case study follows Isabella, a complex premature infant whose Neonatal Intensive Care stay was further complicated by a spontaneous perforation, requiring a laparotomy and bowel resection resulting in faltering growth...