
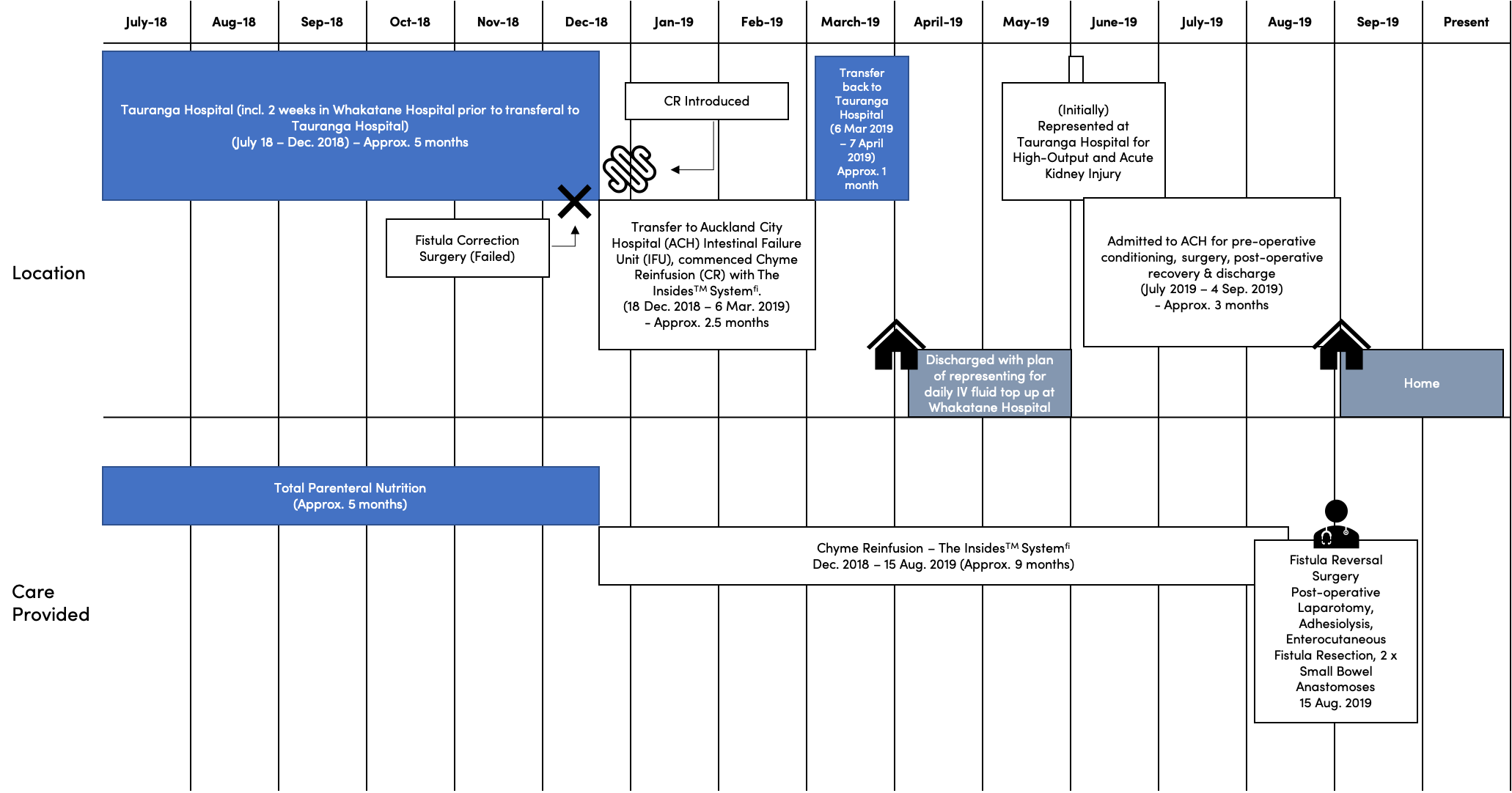
This report presents the case of Ray, a 65-year old male who developed a small bowel enteroatmospheric fistula (EAF) and intra-abdominal sepsis following adhesiolysis surgery for a small bowel obstruction. Ray subsequently spent 5 months in hospital on Total Parenteral Nutrition (TPN) and receiving wound care, while he awaited a fistulotomy. When the surgery failed, Ray was transferred for specialist management at the New Zealand Intestinal Failure Unit, and The Insides® System was introduced to accelerate his recovery.
Prior to this episode, Ray has been fit and active, living with his wife and working as a barber. His previous medical history comprised appendectomy, laparotomy with adhesiolysis, epilepsy, gastroesophageal reflux disease, hypertension, and Peripherally Inserted Central Catheter associated left subclavian vein thrombosis.
At the time of his transfer to the New Zealand Intestinal Failure Unit, Ray had a 15cm x 10cm central abdominal wound encasing the EAF and severe sepsis, with a fistula output of approximately 5L per day, and was dependent on TPN.
Once Ray was stabilized at the Intestinal Failure Unit, Chyme Reinfusion was initiated, using the Insides® System, while he continued TPN.
A contrast plain abdominal x-ray was used to establish the direction of each limb of the fistula and confirm there was no obstruction or distal anastomosis leak before placing a Cook 24 FR tube into the distal limb of Ray’s fistula. The tube remained in situ for the duration of treatment with the Insides® System.
Due to the wound size, an Eakin wound bag was placed over the wound in order to collect the chyme and protect the peristomal skin. The Insides® Pump was attached to the Cook tube and the Pump-Tube assembly was positioned inside the wound bag for immersion in the chyme. Once this setup was complete it was tested by syringing 100mL of water into the bag and activating the Pump via the Driver to verify liquid transportation from the bag, through the Cook tube and into the distal limb of Ray’s bowel.
Chyme reinfusion was slowly commenced with an initial titration period lasting close to a week. Small boluses of chyme starting at 100ml, were reinfused that increased with amount and frequency with tolerance. This was to prime and reinvigorate the down-stream limb and minimise prolonged discomfort and bloating while Ray’s bowel adjusted to being back in continuum.
Once the titration period was completed and Ray was established on chyme reinfusion, a routine for reinfusion and ostomy bag replacement was developed. Reinfusion was performed each time a sufficient amount of chyme had collected in the bag, which was typically around 8 times per day, depending on oral intake. From time to time Ray’s chyme was disposed rather than reinfused - for example if it was too thick to efficiently reinfuse. The bag was changed every day.

Prior to discharge from hospital, Ray received further training and was able to manage all of his reinfusion during the day, completing refeeding approximately every 2 hours. This enabled Ray to return home. At home, Ray continued to reinfuse on his own and with the help of his wife. Although overnight fluid losses were collected in a 2L night bag, Ray was not consistent in refeeding his output each morning, which resulted in him requiring IV fluid top-ups 3 times per week to compensate for night fluid losses not being consistently refed. The Eakin wound bags were changed in clinic every 2 days.
Less than 2 months after discharge from the intestinal failure hospital, Ray re-presented to hospital with high night-time fluid losses through his fistula and an acute kidney injury. Ray was again transferred for specialist care. On review, it was noted that there was an 80cm section of bowel between the two atmospherically exposed loops of bowel that were not receiving any of the reinfused chyme. So, a second Tube and Pump were introduced to ensure luminal exposure to chyme and preserve gut function. This was in place for approximately 2 months leading up to his fistulotomy.

There are multiple benefits associated with Chyme reinfusion in patients with an enterocutaneous and enteroatmospheric fistula. Chyme reinfusion reduces dehydration and the risk of renal impairment through the restoration of electrolyte and fluid balance. Additionally, patients are able to recommence oral nutrition, which enables positive weight gain and the recovery of previously deranged liver enzymes. The ability to gradually wean off from parenteral nutrition reduces the risk of line sepsis commonly associated with the administration of parenteral nutrition through a central venous line catheter as well as reducing the length-of-stay in the hospital, allowing patients to return home earlier. Chyme reinfusion has also been shown to reduce the incidence of post-operative ileus by 17%. Research is currently being conducted, looking into the restoration of the microbiome with chyme reinfusion in comparison to probiotics, initial results are showing an across-the-board increase in bacterial markers of gut health.
In total Ray spent 410 days in hospital over an 18-month period. Much of this time was prior to introduction of chyme reinfusion using the Insides® System. It only took 4-months from commencing treatment with the Insides® System. for Ray’s enterocutaneous fistula output to reduce to 1-2L per day. During this time, Ray was able to gradually wean off Total Parenteral Nutrition as he recommenced oral nutrition within the first month.
After 9 months of using the Insides® System, Ray underwent surgery to successfully resect his fistula and restore his bowel continuity. Ray required 2 weeks of TPN prior to his fistulotomy to ensure he had good protein reserves for a successful surgical recovery.
This case study demonstrates that the Insides® System for chyme reinfusion is an effective way to maintain nutrition and hydration and preserve intestinal function in patients with enterocutaneous fistula while reducing their ongoing requirement for parenteral nutrition. The Insides® System enables reinfusion to be completed cleanly and efficiently by patients and their caregivers and provides a viable treatment option to accelerate recovery and improve quality of life in patients with enterocutaneous fistula.
Individual results may vary. Testimonials do not claim to represent typical results. All testimonials are received from real patients via text, in person, or through video submission, and may not reflect the typical patient experience. Testimonials are not intended to represent or guarantee that anyone will achieve the same or similar clinical results. Each patient’s condition is unique to their physiology and health status. Thus, the testimonials shared by The Insides Company may not reflect the typical patient experience.

This case study follows Jaybie, a preterm infant born with gastroschisis who required multiple abdominal surgeries and experienced a complex postoperative course. She developed intestinal failure, became dependent on intravenous nutrition, and faced a long and challenging path to discharge...

This case study follows Isabella, a complex premature infant whose Neonatal Intensive Care stay was further complicated by a spontaneous perforation, requiring a laparotomy and bowel resection resulting in faltering growth...